The Department of Orthopaedic Surgery has both trauma specialists and microsurgeons who have the ability to manage very complex cases. The management of these patients typically requires multidisciplinary care that benefits from coordination with specialists from general surgery, plastic surgery and spine.
Our dedicated nursing staff helps coordinate patient access and navigation through the Keck Medicine of USC health system. Physiotherapy is a key component of orthopaedic care and is delivered by therapists with a breadth of specialty clinical expertise.
Surgeons at Keck Medicine of USC are leading authorities in reconstructive microsurgery. Our highly skilled team members are experts in managing complex wounds using techniques such as free flaps, rotational flaps and vascularized bone grafts. We can perform vascular repair down to 400-µm-diameter vessels. We can also transfer muscle tissue from the lower extremities or upper body to close a tissue defect and restore function.
Vascularized bone grafts are able to bridge almost any bony defect in the upper or lower extremity that is caused by trauma, infection or a tumor. (See case study below.) The defects can be up to 20 cm in length and the grafts can comprise bone, muscle and/or skin as necessary to cover the defect.
A 12-year-old male sustained sub-total amputation of his left forearm with a washing machine. The only structure that was not lacerated was the ulnar nerve. A multidisciplinary team of orthopaedic surgeons and microvascular surgeons was rapidly assembled and the patient underwent surgery. Internal fixation was used to address the bone fractures, and the ulnar artery was grafted with a reversed saphenous vein graft. The microvascular team repaired all vessels, which can be particularly challenging given the smaller diameter vessels in pediatric patients.
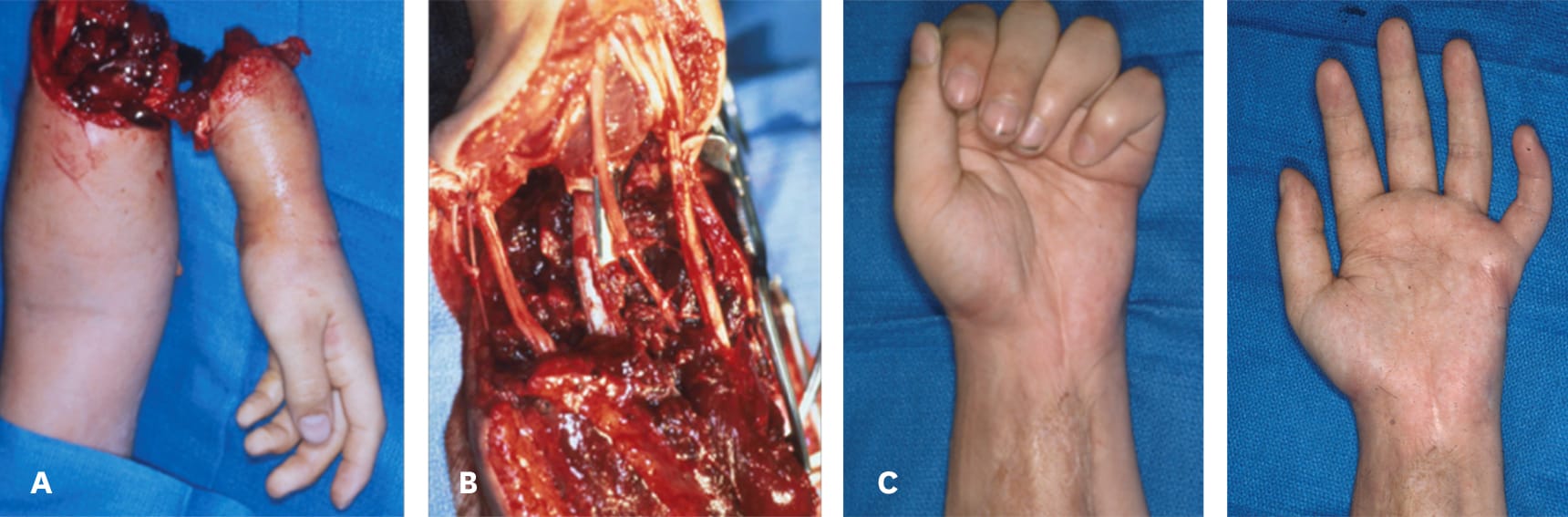
A 12-year-old patient with (a) sustained sub-total amputation of his left forearm. (b) Revascularization and repair with internal fixation. (c) Free muscle flap covering the soft tissue defect on the anterior side of the forearm.
All nerves were repaired and a free muscle flap was used to cover the soft tissue defect on the anterior side of the forearm and restore wrist and finger flexion. The patient regained function after one year with a 40-pound grip strength. The affected arm is one inch shorter than the opposite arm.
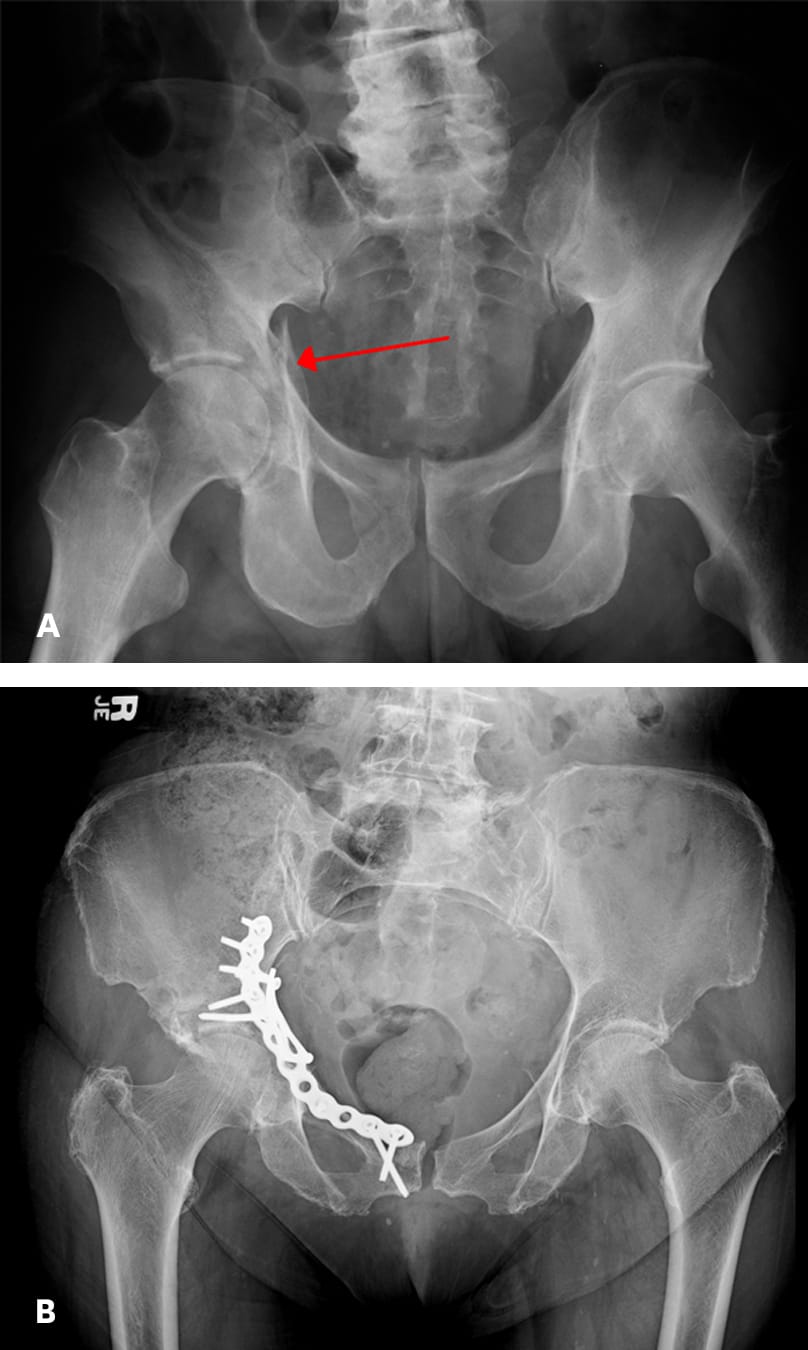
(a) Acetabular fracture
(b) Acetabular fracture fixed with screws
Acetabular fractures can be simple or complex; it is crucial for patients to receive individualized care to maximize outcomes. Anatomic reduction of the joint surface is key; this minimizes the chance that the patient will develop arthritis of the hip joint. To achieve optimal outcomes for patients, the surgeons and staff at USC Orthopaedic Surgery provide dedicated expertise in acetabular fractures.
Keck Medicine of USC offers minimally invasive and percutaneous approaches for acetabular surgery. These options include the use of an anterior intrapelvic approach and a pararectus approach, which can be particularly beneficial for injury patterns often seen in elderly patients. Percutaneous fixation of the acetabulum can be used for minimally displaced fractures and patients who cannot tolerate open surgery, with the benefit of an earlier return to ambulation after surgery.
Tibia fractures are another area of expertise at USC Orthopaedic Surgery. Many of these fractures are open fractures, and patients may have large defects in skin, muscle or bone as a consequence. Tibia fractures typically heal more slowly than other bone fractures and are more prone to becoming a non-union. Our fracture specialists have extensive experience managing complex tibia fractures to mitigate these challenges. Large defects in the tibia can be addressed with bone grafting or bone transport, as appropriate, and soft tissue problems may be treated with a variety of local and free flaps.

Our physicians also build upon translational research being conducted in laboratories at Keck School of Medicine of USC, specifically to better understand bone healing and use newer technologies. For instance, investigators are examining new ways to debride fractures and how different methods for rod insertion affect the risk of complications.1-3