Our multidisciplinary team includes neurosurgeons, with specialties in open vascular surgery and endovascular neurosurgery, vascular neurologists and neurocritical care physicians. The wide array of skills represented in these team members allows us to offer an extensive range of treatments for all forms of ischemic stroke and hemorrhagic stroke. Our team meets in weekly conferences to discuss cases and come to a consensus on treatment. We are one of the highest-volume centers for stroke treatment in the region and perform several hundred operations annually for aneurysms, vascular malformations, ischemic stroke and other cerebrovascular diseases.
The Roxanna Todd Hodges Comprehensive Stroke Clinic offers a multidisciplinary evaluation of patients for stroke and transient ischemic attack. The clinic specializes in evaluating and treating rare and complicated cerebrovascular disorders. A multidisciplinary team of vascular neurologists, occupational therapists, physical therapists and speech therapists staffs the clinic. The clinic also specializes in rapid evaluation of Transient Ischemic Attack (TIA). State-of-the-art care is combined with cutting-edge research on novel biomarkers and advanced neuroimaging for stroke. Patients are referred back to their community physician to continue care once their acute needs are met at USC Neurosciences.
The USC Revascularization Center is a multidisciplinary collaboration including the departments of neurosurgery, neurology and plastic surgery. It is the largest revascularization center in Southern California, specializing in the diagnosis, medical and surgical treatment of complex cerebrovascular diseases, including Moyamoya disease, intracranial atherosclerosis, complex aneurysms and idiopathic occlusive disease. This collaborative effort has won national recognition from the American Society for Reconstructive Microsurgery at the 2016 Annual Meeting.1 Through interdisciplinary microsurgical collaboration, creative solutions to difficult problems are possible. Additionally, combined approaches to treat intracranial pathology, such as the “eyelid” craniotomy, can allow for improved cosmetic outcomes for even complex pathology.2
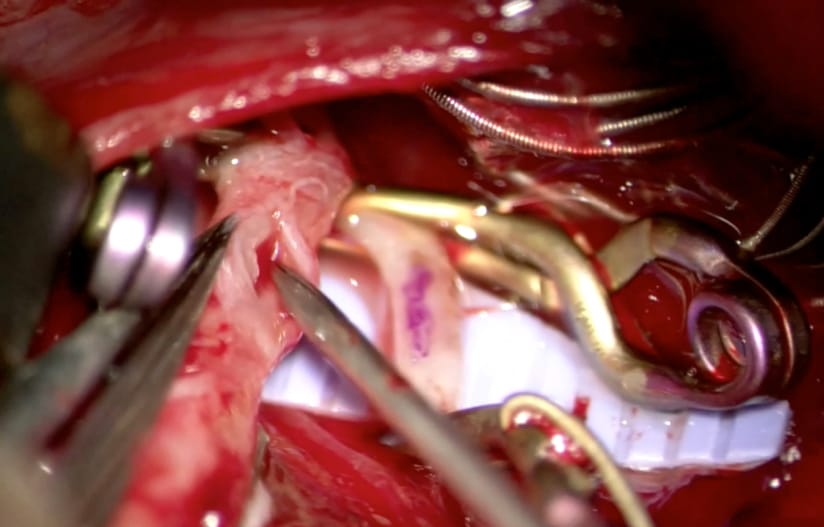
Figure 1 – An intraoperative, microscopic view of preparations being made for a side-to-side bypass from the patient’s radial artery graft to a frontal middle cerebral artery branch. This case was awarded “Best Case Selections” by the American Society for Reconstructive Microsurgery.1
Additional, specialized resources for stroke care at Keck Medical Center of USC include a neurocritical care unit in the ICU, which houses dedicated physicians and nurses with expertise in stroke treatment. We also offer stroke support groups to help stroke survivors obtain information and network with each other.
One of the most important factors in a patient’s outcome after a stroke is the time to treatment. That is why Keck Medicine of USC has built a rapid transfer service for patients needing treatment at Keck Medical Center of USC. Through the Rapid Transfer hotline, referring physicians can speak with an attending physician in cerebrovascular neurology for an immediate conversation any time of the day or night. After the conversation, our team can dispatch an ambulance and expedite the patient transfer to Keck Hospital of USC. Our stroke team is waiting and ready as the patient arrives at the hospital to ensure that critical minutes are not wasted. In 2016, Keck Hospital received 752 neuroscience transfers through our Rapid Transfer hotline. To learn more about the rapid transfer hotline, call (800) USC-CARE.
Tele-stroke evaluation is available from physicians at USC Neurosciences to hospitals that don’t have the staff to support a neurological evaluation in person. Research has shown that tele-stroke programs are beneficial to rural hospitals.3 The implementation of the USC Telestroke program in several community hospitals has enabled these hospitals to become Primary Stroke Centers. Through the Telestroke program, the Keck Medical Center of USC hopes to improve stroke care in the community by building a true spoke-and-hub model of care. This model provides acute expert stroke consultation to build local community primary stroke care, while offering tertiary stroke care at Keck Medical Center for complex cases. Referring physicians can learn more about this service by contacting Mirabai Chuldenko, RN, BSN, stroke coordinator at Keck Hospital of USC, at (323) 865-1671.
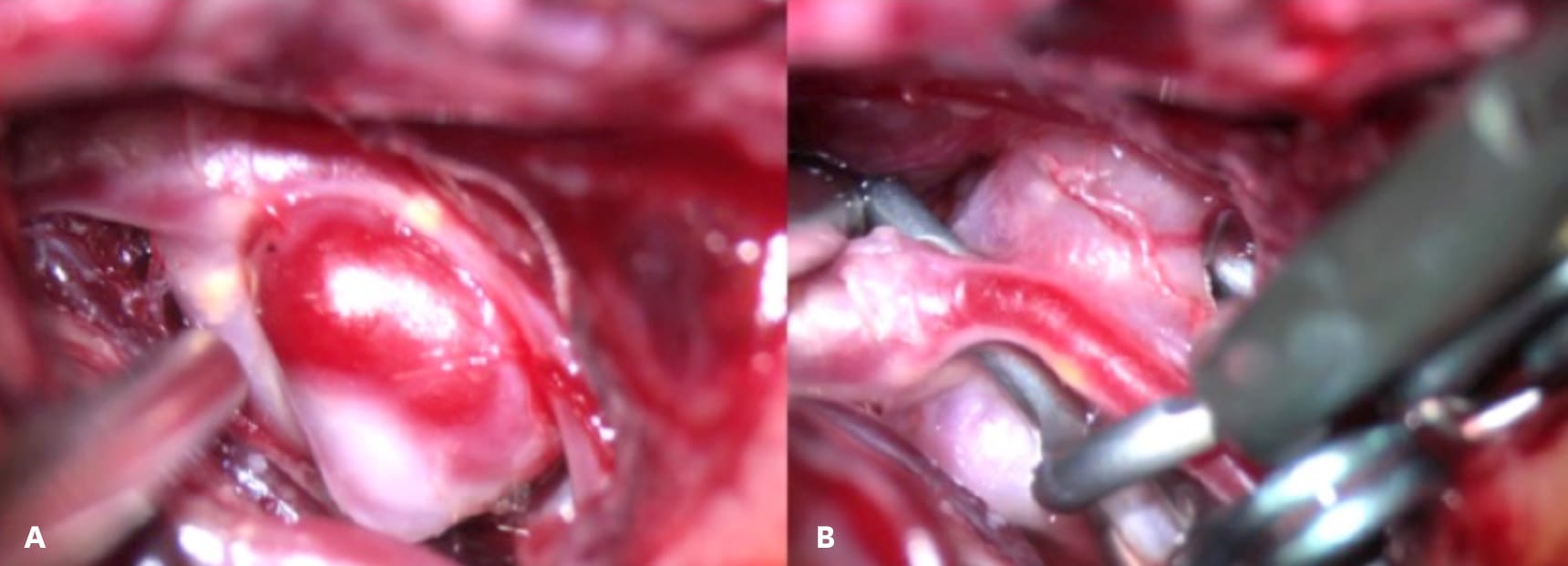
Figure 2 – (a) An intraoperative photo of an unruptured cerebral aneurysm prior to clipping. (b) An intraoperative photo of the same aneurysm during a complex clip reconstruction.
In addition to the comprehensive treatment for acute stroke, we have a robust program focusing on stroke prevention. Stroke prevention is focused around five areas: controlling blood pressure, cholesterol and blood sugar; managing antithrombotic medications and promoting an active lifestyle. We offer excellent stroke educational programs for patients and caregivers, including a monthly stroke support group. We offer carotid endarterectomy or carotid stenting for patients with carotid stenosis. We also aim to mitigate stroke risk for patients with non-ruptured aneurysms or vascular malformations.
Our robust patient care is complemented by our depth of experience in clinical trials. Keck Medicine of USC is one of 25 national stroke center sites for StrokeNet, an NIH-funded network conducting clinical trials and translational research to advance acute stroke treatment, stroke prevention, recovery and rehabilitation (see article on Clinical and Translational Research).